Unit 2 – Medial Tibial Stress Syndrome (Shin Splints) (Preview)
Quiz: When you have completed the learning requirements for this unit, you will be able to access its quiz by clicking on the link found at the bottom of this web page. You can attempt the quiz as many times as you need to achieve a pass mark of at least 70%.
Disclaimer: Please read the Disclaimer at the bottom of this page.
Copyright © Educom Pty Ltd: All material on this website (including the text, graphics, videos and downloadable files) is owned by or licensed to Educom Pty Ltd and is subject to copyright and other intellectual property rights under international conventions.
How to Complete This Unit
This unit consists of reading material, video presentations, and practice resources. When you have completed the learning material in this unit, you will be able to access its multiple-choice quiz by clicking on the link found at the bottom of this web page. You can attempt the quiz as many times as you need to achieve a pass mark of at least 70%.
Unit Credit: 2 Hours
2 hours include allocated time for progressing through the reading material, watching the videos, considering the reflection points, final review of the unit and completing the quiz.
Content Links
The following buttons can be used to navigate the content in this unit.
Diagnostic Features
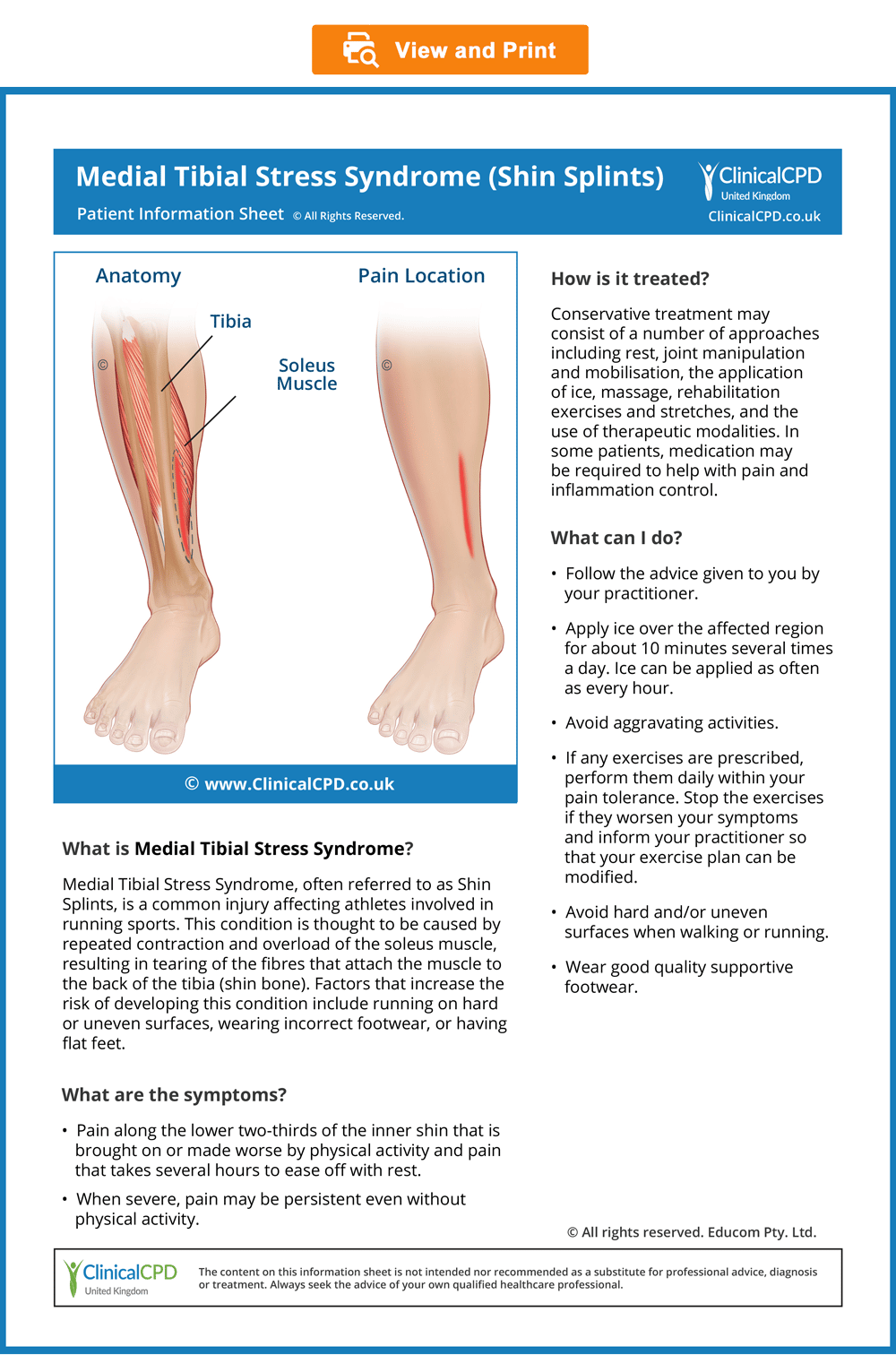
Medial Tibial Stress Syndrome
(Shin Splints)
Introduction
Definition and Causes
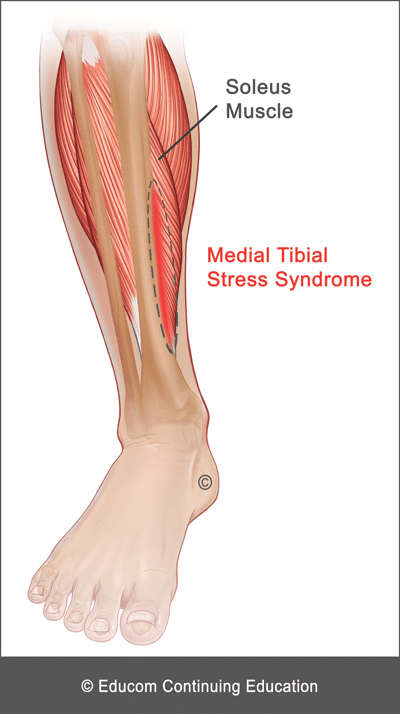
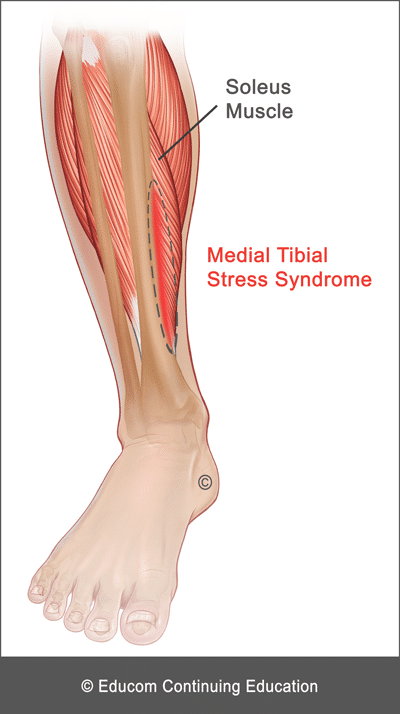
Medial Tibial Stress Syndrome (MTSS), often referred to as “shin splints”, causes pain along the distal two-thirds of the medial tibial border. It is a common injury affecting athletes involved in running sports. Health practitioners need to differentiate MTSS from stress fractures and, more importantly, from Chronic Exertional Compartment Syndrome. Another lower leg syndrome of great importance is Acute Compartment Syndrome which is typically caused by local trauma (e.g., fracture of the tibia) resulting in acute loss of blood flow, constituting a medical emergency.
The pathophysiology of MTSS is thought to be a traumatic periostitis of the tibia involving the tendinous attachments of the soleus (primarily), flexor digitorum longus, and posterior tibialis, with tearing of Sharpey’s fibres at their bony insertion.
Risk Factors
- Obesity
- Female gender
- Excessive pronation
- Muscle dysfunction
- Incorrect footwear
- Running on hard or uneven surfaces
- Significant increase in running distance
- Fatigue
- History of previous tibial stress fractures
- Vitamin D deficiency and lower bone mineral density
- Leg length deficiency
History and Presentation
- Exercise-induced diffuse pain along the posteromedial border of the distal two-thirds of the tibia
- Pain exacerbated by physical activity (e.g., running)
- Pain eases off with rest after several hours but may persist longer
- Absence of leg muscle tenseness, cramping, burning pain and numbness/tingling in the foot
Physical Examination
- Diffuse tenderness along the distal two-thirds of the posteromedial tibial border (focal tenderness should alert the examiner to the possibility of a stress fracture)
- Absence of tenseness in the leg compartments (compartment tenseness is a feature of Acute or Chronic Exertional Compartment Syndrome)
- Normal distal pulses and an absence of severe swelling, erythema, or numbness
Diagnostic Imaging
Medial Tibial Stress Syndrome is usually a clinical diagnosis with imaging typically used to help rule out other conditions. However, if diagnostic imaging is to be used, MRI is considered the most sensitive modality.
To rule out stress fractures, plain radiography is considered to have poor sensitivity while MRI is considered to be the most sensitive modality for detecting stress fractures.
Red Flags
The following are examples of “red flags” for patients presenting with leg pain:
- History of a significant injury
- Severe or focal pain
- Unrelenting pain
- Nocturnal pain
- Unexplained weight loss
- Fever
- Deformity
- Significant swelling
- Leg pain arising after a prolonged period of immobility or bed rest
- Presence of tingling, numbness, burning or other neurological impairment
- Loss of distal leg pulses
- Significant loss of range of motion
- Severe tenderness on palpation or severe pain with any examination procedure
If any “red flags” are identified during history taking and clinical examination, referral for urgent medical evaluation and further investigation is warranted.
Management
If no red flags are identified or further investigations do not reveal any contraindications to treatment, management of the condition may begin.
The suggested conservative therapy, home advice, and clinical tips in this section are based on published materials and the clinical experience of the authors of this course. This should not be interpreted as a prescriptive guide to the treatment of this or any other condition. The use of this content is subject to the “Disclaimer” found at the bottom of this web page.
Conservative Therapy
- Correction of joint dysfunction along the kinetic chain with emphasis on the knee, ankle, and pelvis
- Correction of gait and other biomechanical factors
- Electrotherapeutic modalities (e.g., ultrasound and extracorporeal shockwave)
- Massage
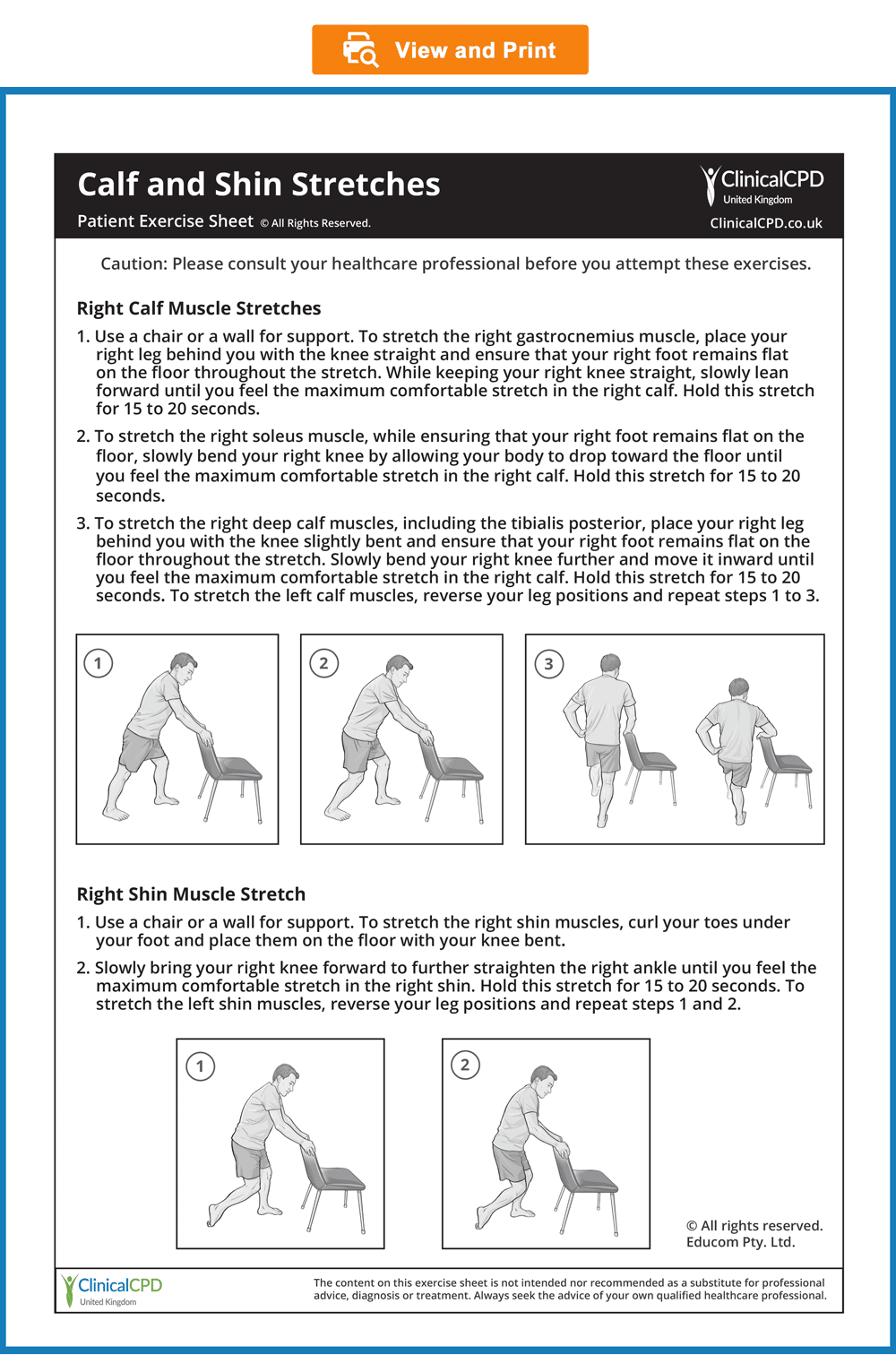
- Rehabilitation exercises and stretches
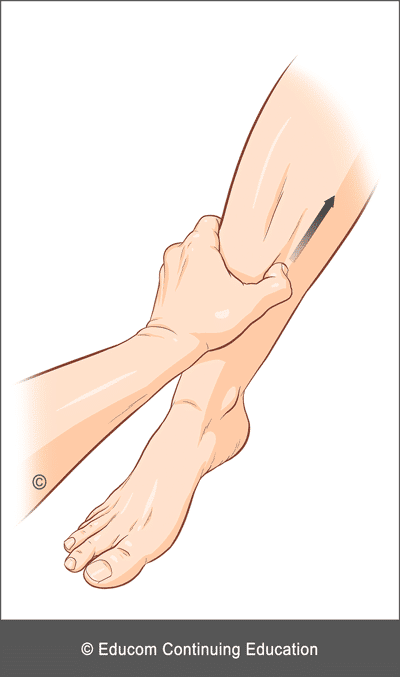
- Massage – With regard to massage, one approach is to use your thumb to apply pressure over the most distal part of the painful area and then sweep upwards. Typically the patient will report that the pain eases after several sweeps.
Home Advice
- Apply ice over the affected region for about 10 minutes, several times a day for pain control. Ice can be applied as often as every hour.
- Avoid aggravating activities.
- When pain allows, perform your prescribed exercises followed by stretches (see Patient Exercise Sheets below).
- When it is time to resume activities (e.g., running), avoid hard and/or uneven surfaces.
- Runners should begin with short distances and gradually increase the distance over time.
- Wear good quality supportive footwear.
- Ice versus Heat – Some practitioners advocate the use of moist heat in the subacute or chronic phase. However, we have found that patients often benefit from the continued application of ice to reduce discomfort as they engage in more activities to restore a full and pain-free joint function.
- Rehabilitation Exercises – It is recommended that strengthening exercises be performed, followed by stretching.
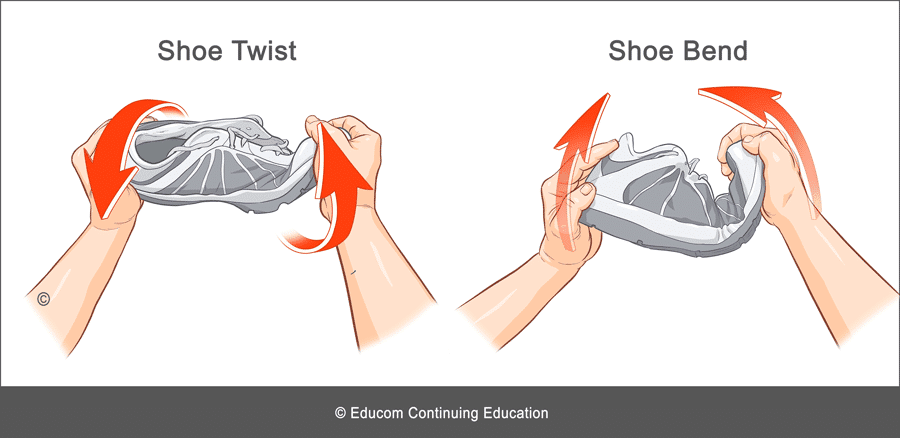
- Supportive Footwear – To maintain good support, footwear should be replaced at regular intervals. The patient should avoid footwear that is very flexible because it will not provide adequate support. Two simple tests to check the level of support provided by the footwear can be performed (Shoe Twist and Shoe Bend).
- Shoe Twist: Hold the shoe at both ends and twist it. If the shoe twists too easily it will not provide adequate support.
- Shoe Bend: Hold the shoe at both ends and fold it upward. If the shoe bends too easily it will not provide adequate support.
For Patients
Patient Information Sheet
- Provide information to the patient about their condition to improve their understanding and enhance compliance (see the downloadable ready-to-use Patient Information Sheet below).
- In our experience, patients who are well informed about their condition are more likely to comply with the recommended management strategy, achieve good outcomes, become loyal patients, and recommend their family and friends to seek treatment.
- To view, download or print the Patient Information sheet, simply click on the image below.
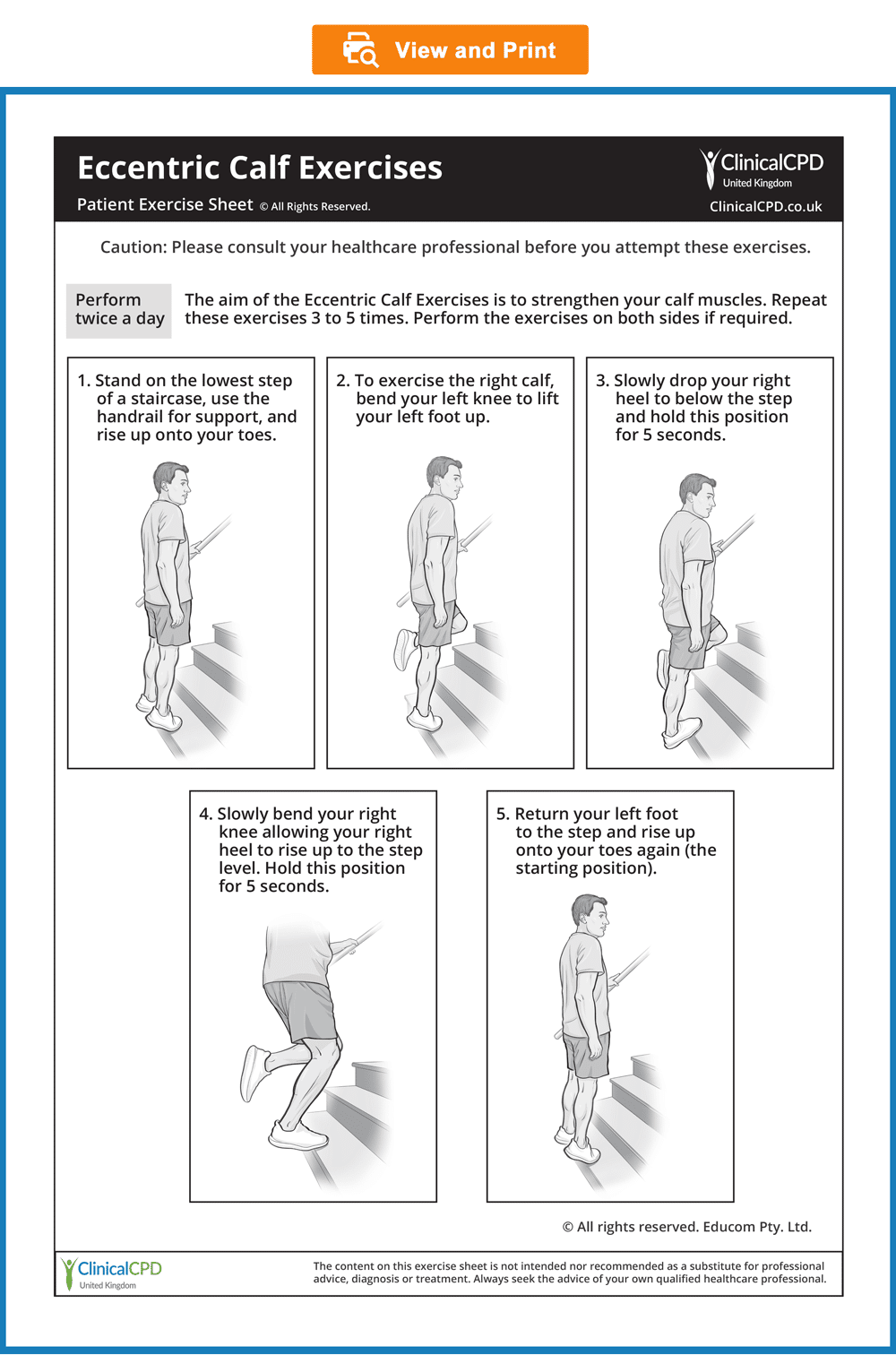
Patient Exercise Sheets
- When appropriate, the patient should gradually begin doing exercises at home.
- Always recommend warm-up activities before commencing specific exercises. Warm-up activities include simple limbering movements or prescribed strength exercises at light loads.
- Instruct your patients to perform their strengthening exercises before they perform their stretches.
- Always instruct your patients to use caution when performing their rehab exercises in order to avoid overloading, overstretching, or any undue pain.
- Emphasise that they should stop any exercises that cause them concern and seek your advice at the earliest opportunity
- To view, download, or print the Patient Exercise Sheets, simply click on the images below.
Optimise Your Diagnostic Reasoning
Our Recommended Approach
To help you sharpen your diagnostic reasoning skills, we recommend the following steps:
- Step 1: In the following case scenario, read through the provided patient information in each section.
- Step 2: Consider the ‘Diagnostic Reasoning Question’ for that section and take some time to think about your response before you read our suggested answer.
- Step 3: To encourage critical thinking, we recommend that you first attempt to answer the question on your own. If you wish, you can hide our suggested answer by clicking on the ‘Suggested Answer’ arrow. When ready, click the arrow again to reveal our answer and compare it with your own.
Please note that the suggested answers are only indicative and not exhaustive. They serve as guidelines and should not be considered complete answers.
Patient’s History
In the sections below, you are provided with case history information. The material presents a systematic approach to performing a focused and relevant case history in order to narrow down the possible causes of the patient’s complaint. As you read the following material, you are encouraged to answer the questions posed to test your diagnostic reasoning skills.
Who is the patient and where is the pain?
When was the onset and what caused the onset?
David is a 30-year-old university lecturer who presents with a primary complaint of right lower leg pain. He points to the lower two-thirds of the medial tibial border as the site of his pain. He believes it is related to running, which he began about six months ago when he decided to train for his first marathon. The pain has gradually developed over the last three months and seems to have coincided with an increase in his training distances.

|
What differential diagnoses would you consider for David? |
Suggested Answer
His description of lower leg pain can indicate the possibility of several conditions, including:
- Medial lower leg muscle strain
- Tibial stress fracture
- Medial tibial stress syndrome
- Chronic exertional compartment syndrome
- Foot or ankle joint dysfunction
|
How does David’s recent increase in training distances, which coincides with increased pain, inform the diagnostic process? |
Suggested Answer
The correlation between his recent increase in training distances and increased pain provides critical insights into the diagnostic process:
- Overuse Injuries – Overuse injuries are characterised by a gradual onset of pain that worsens with increased running distance. Conditions such as medial tibial stress syndrome (“Shin Splints”), stress fractures, or tendinitis are commonly associated with repetitive stress and overuse.
- Medial Tibial Stress Syndrome – Pain along the medial tibial border, particularly in runners who have recently increased their mileage, is a hallmark of medial tibial stress syndrome (“Shin Splints”). This condition results from repeated stress on the tibia and surrounding muscles, often due to increased activity levels without adequate conditioning or rest.
- Stress Fractures – The progression of pain that coincides with increased activity raises concern for a stress fracture, especially if the pain is persistent and focal. Stress fractures can develop when bones are subjected to repetitive loading without sufficient recovery, leading to microdamage.
What are the pain characteristics?
What are the aggravating and relieving factors?
What has been the course of the pain?
David describes his pain as a diffuse ache, rating it 7 out of 10 in intensity at its worst. He notes that the pain is aggravated by running and gradually subsides over several hours with rest. He reports that the pain has progressively worsened with increased running distance. Currently, even simple daily activities such as walking and climbing stairs can be painful.
|
How does the presence of shin pain that is aggravated when running and gradually subsides over several hours with rest inform the diagnostic process? |
Suggested Answer
- Medial Tibial Stress Syndrome – Shin pain takes several hours to ease off after running.
- Chronic Exertional Compartment Syndrome – Shin pain often disappears within 10 to 20 minutes after the activity has ended.
- Stress Fracture – Shin pain usually continues after running and can persist even during rest.
Are there any associated symptoms?
Upon further questioning, David reports that he does not experience any associated symptoms, such as numbness or tingling.
|
What is the diagnostic significance of the absence of associated symptoms such as numbness or tingling in a patient with shin pain? |
Suggested Answer
The absence of associated symptoms such as numbness or tingling in a patient with shin pain supports a diagnosis of a musculoskeletal condition and makes neurological or vascular conditions less likely.
Is there a past history that is relevant to the current complaint?
David has no previous history of similar complaints. He reports having suffered a right ankle sprain in his early twenties.
|
How does his past history inform the diagnostic process? |
Suggested Answer
The absence of a previous history of similar complaints suggests that this is a new condition strongly linked to his running. His previous right ankle sprain raises the possibility of persistent ankle joint dysfunction, which may be causing or contributing to his current complaint.
Are there any red flags?
The patient is asked the following questions to identify any red flags that could indicate serious pathology. Even if the patient has already provided information in the case history that relates to these questions, it is recommended that they be readdressed to ensure a thorough exploration.
- Do your symptoms disappear even for a short time? “Yes, it gradually disappears after I finish a run.”
- Does the pain wake you up at night? “No.”
- Do you feel weak in your legs? “No.”
- Have you recently had any fever, chills, or night sweats? “No.”
- Have you recently had an infection or other illness? “No.”
- Do you have a history of cancer, inflammatory arthritis, or fracture arising from minor trauma? “No.”
|
Do any of David’s answers raise a red flag? |
Suggested Answer
None of his responses suggests a red flag.
What is the list of possible causes for the patient’s complaint?
|
How would you rank the differential diagnosis list based on the available history? |
Suggested Answer
- Medial tibial stress syndrome
- Tibial stress fracture
- Chronic ankle dysfunction
- Medial lower leg muscle strain
- Chronic exertional compartment syndrome
Reflection Point
Please stop and take a moment to consider whether the main requirements of an adequate and relevant patient history taking have been fulfilled. Are there any additional questions you would have asked and, if so, why?
Before the physical examination findings are presented below, please reflect on what physical examination procedures you would perform to adequately evaluate this patient.
Performing Physical Examination
In the sections below, you are provided with physical examination findings for this patient. The material presents a systematic approach to performing a focused and relevant physical examination to narrow down the possible causes of the patient’s complaint. You are encouraged to answer the questions posed to test your clinical reasoning and diagnostic skills as you read the following material. As you read the following material, you are encouraged to identify whether the essential elements of the physical examination have been adequately covered.
Vital Signs
David’s vital signs are within normal limits.
|
What do normal vital signs mean? |
Suggested Answer
Normal vital signs typically indicate that there are no immediate life-threatening conditions present. Normal temperature, in particular, indicates the absence of acute infection.
Inspection
Inspection of the right lower leg is normal, with no evidence of swelling or erythema. However, inspection of his feet and ankles reveals bilateral pes planus.
|
How does the absence of swelling or erythema inform the diagnostic process? |
Suggested Answer
Swelling and erythema are common in acute inflammatory or infectious conditions, while their absence points toward chronic overuse issues or biomechanical problems.
|
How does the finding of bilateral pes planus contribute to the diagnostic process? |
Suggested Answer
Pes planus (flat feet) can contribute to improper biomechanics during running, leading to increased stress on the tibia and surrounding structures. Pes planus often results in excessive pronation, which can increase the load on the medial aspect of the tibia, contributing to conditions like medial tibial stress syndrome.
Range of Motion
Assessment of his right ankle and knee range of motion is normal.
|
What is the significance of a normal range of motion assessment for the right ankle and knee in the context of David’s shin pain? |
Suggested Answer
Overuse injuries, such as medial tibial stress syndrome, often occur with normal joint range of motion but present with pain due to repetitive stress and inflammation. In contrast, joint pathologies such as ligament tears, significant cartilage damage, or arthritis would typically present with a restricted range of motion. The normal range of motion in David suggests that there are no significant joint restrictions, ligamentous injuries, or major structural abnormalities in his ankle and knee.
Palpation
On palpation, diffuse tenderness is present along the distal two-thirds of the posteromedial tibial border. There is no evidence of increased tension in the anterior compartment of the right leg. Normal dorsalis pedis and posterior tibial pulses are present. A functional assessment of the foot and ankle joints reveals no abnormalities.
|
How does the presence of diffuse tenderness, as opposed to localised tenderness, inform the diagnostic process? |
Suggested Answer
Diffuse tenderness along the tibia is consistent with a diagnosis of medial tibial stress syndrome. In contrast, a stress fracture typically presents with focal tenderness.
|
How does the absence of increased tension in the anterior compartment of the right leg inform the diagnostic process? |
Suggested Answer
The absence of increased tension helps rule out Chronic Exertional Compartment Syndrome. This condition is characterised by increased pressure within a muscle compartment, leading to pain, tightness, and neurological symptoms.
|
How do the normal dorsalis pedis and posterior tibial pulses inform the diagnostic process? |
Suggested Answer
Vascular conditions (e.g., peripheral artery disease) typically present with diminished or absent pulses, which can lead to ischaemia and pain during activity. David’s normal pulses indicate that there is no significant vascular compromise in his lower extremities.

Reflection Point
Given the patient’s history and examination findings up until this point, please stop and take a moment to consider which special tests should be performed to further evaluate this patient.
Special Tests
The External Rotation Stress test is performed and is negative, with no reproduction of David’s pain or evidence of joint instability.
|
What is the External Rotation Stress test designed to assess, and what do his normal results suggest? |
Suggested Answer
The External Rotation Stress test is designed to detect the involvement of the ankle syndesmosis. This negative result helps to rule out dysfunction of this joint as a cause or contributing factor for his condition.
For a demonstration of how the External Rotation Stress test can be performed, please watch the video below.
The Heel Tap test is performed and is found to be negative.
|
What is the Heel Tap test designed to assess? |
Suggested Answer
The Heel Tap test is designed to detect fractures in the lower extremity. A negative result suggests the absence of a fracture.
For a demonstration of how the Heel Tap test can be performed, please watch the video below.
The Ankle Anterior Drawer and Talar Tilt tests are performed and found to be negative.
|
What are the Ankle Anterior Drawer and Talar Tilt tests designed to assess? |
Suggested Answer
The Ankle Anterior Drawer and Talar Tilt tests are designed to detect ankle instability. David’s negative results help rule out ankle instability as a cause or contributing factor.
For a demonstration of how these tests can be performed, please watch the videos below.
Reflection Point
Please stop and take a moment to consider whether all the elements of an adequate and relevant physical examination have been completed for this patient. Are there any additional procedures you would have performed and, if so, why?
Clinical Diagnosis
Based on the available information, what is the most likely clinical diagnosis?
Suggested Answer
Medial Tibial Stress Syndrome.
References and Suggested Further Readings:
C. Menéndez et al. Medial Tibial Stress Syndrome in Novice and Recreational Runners: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 7457.
M. Winters et al. Medial tibial stress syndrome can be diagnosed reliably using history and physical examination. Br J Sports Med. 2018 Oct;52(19):1267-1272.
R. Galbraith and M Lavallee. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med (2009) 2:127–133.
L. Callahan. Overview of running injuries of the lower extremity. www.uptodate.com
Disclaimer: The Clinical CPD™ website (including the text, graphics, downloadable resources, and videos that appear on clinicalcpd.co.uk) is designed to offer users general health information for educational purposes only. The general health information provided on this site is not intended to replace personal consultation with a qualified healthcare professional. Always seek the advice of a healthcare professional for questions related to your disease, disease symptoms, and appropriate treatment.
Copyright © Educom Pty Ltd: All content on this website, including text, graphics, videos, and downloadable files, is the property of Educom Pty Ltd and is protected by copyright and other intellectual property laws under international conventions. Unauthorized use or duplication of this material without express written permission from the site’s author or owner is strictly prohibited.
Quiz: This concludes the learning material for this unit. You may review the material or take the multiple-choice quiz for this unit now or at a later time. The quiz for this unit must be completed before you can access the next unit in this course. You can attempt the quiz as many times as you need to achieve a pass mark of at least 70%.
To take the quiz click the button below.