Quiz: When you have completed the learning requirements for this unit, you will be able to access its quiz by clicking on the link found at the bottom of this web page. You can attempt the quiz as many times as you need to achieve a pass mark of at least 60%.
Disclaimer: Please read the Disclaimer at the bottom of this page.
Copyright © Educom Pty Ltd: All material on this website (including the text, graphics, videos and downloadable files) are owned by or licensed to Educom Pty Ltd and is subject to copyright and other intellectual property rights under international conventions.
How to Complete This Unit
This unit consists of reading material, video presentations, and practice resources. When you have completed the learning material in this unit, you will be able to access its multiple-choice quiz by clicking on the link found at the bottom of this web page. You can attempt the quiz as many times as you need to achieve a pass mark of at least 60%.
Unit Credit: 2 Hours
2 hours include allocated time for progressing through the reading material, watching the videos, considering the reflection points, final review of the unit and completing the quiz.
Content Links
The following buttons can be used to navigate the content in this unit.
Diagnostic Features
Sternoclavicular Joint Sprain
Introduction
Sternoclavicular joint injuries involve the sternoclavicular joint and its associated ligaments and can be of a traumatic or atraumatic aetiology. Traumatic injury to the sternoclavicular joint is reported to be caused most commonly by motor vehicle accidents or sporting trauma. The mechanism of injury is said to be that of compression force to the lateral shoulder, together with a vector that drives the medial end of the clavicle anteriorly or posteriorly, typically resulting in a sprain of the joint. When the injury is severe dislocation may occur. In cases of atraumatic injury, the usual mechanism is sustained activity with the arm in an elevated position.
With only half of the medial end of the clavicle in direct contact with the manubrium, the sternoclavicular joint is an inherently unstable joint relying on ligamentous support. The joint contains an intra-articular disc which acts as a shock absorber and allows for a greater range of mobility.
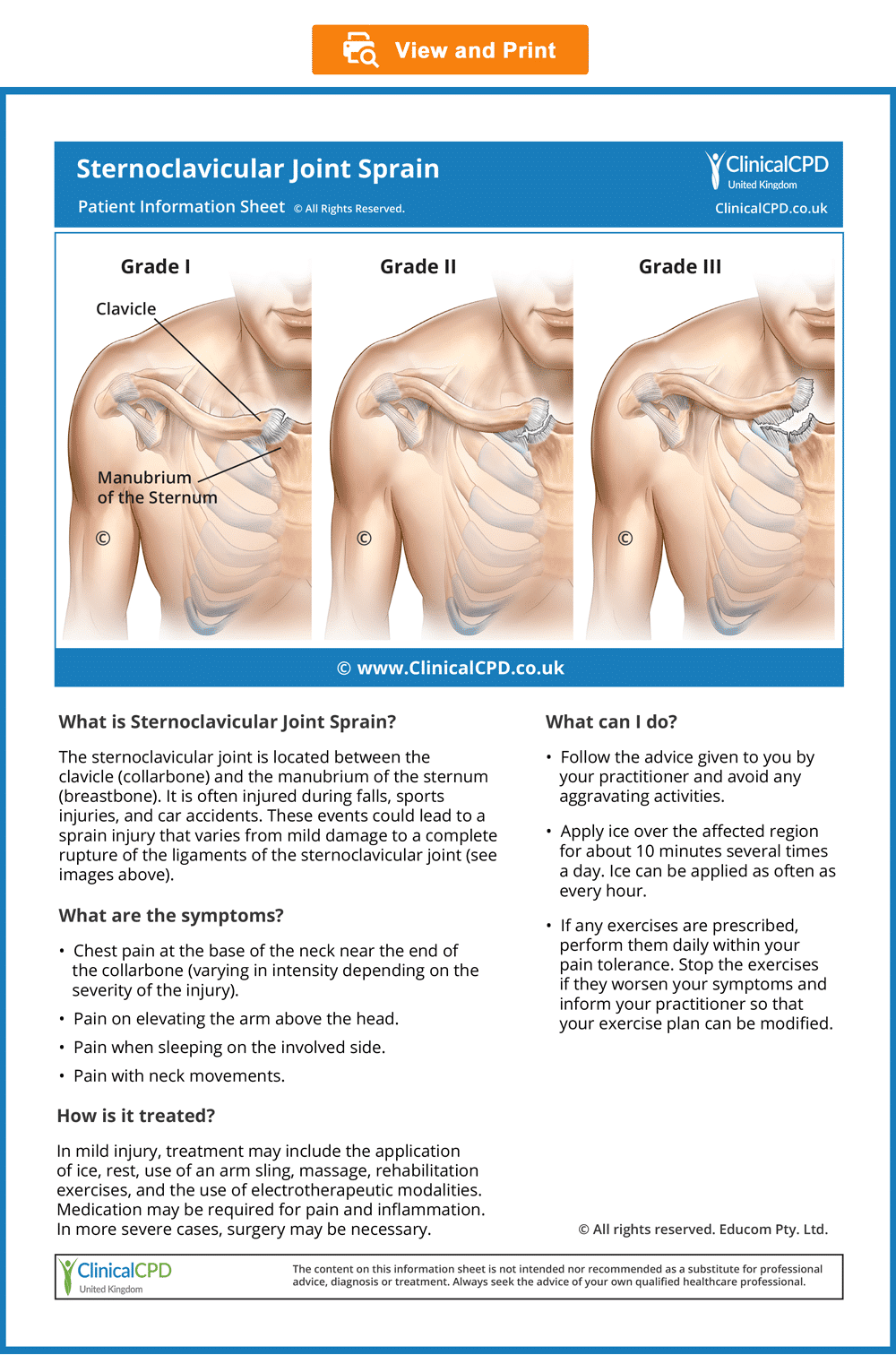
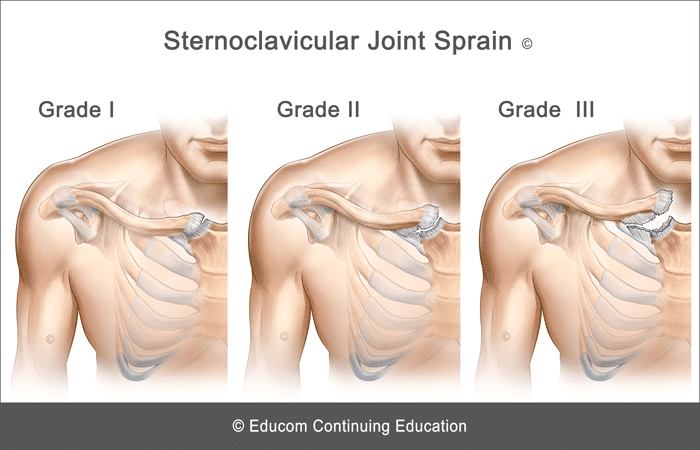
Injuries of the sternoclavicular joint are classified into three types based on their severity:
Grade I – Sprain: An incomplete tear or stretching of the sternoclavicular and costoclavicular ligaments.
Grade II – Subluxation: A complete tear of the sternoclavicular ligament but only a partial tear of the costoclavicular ligament.
Grade III – Dislocation: A complete rupture of the sternoclavicular and costoclavicular ligaments.
History and Presentation
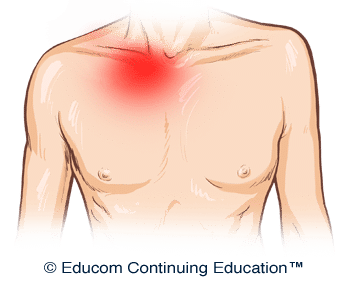
- Anterior chest pain primarily localised to the sternoclavicular joint
- Pain aggravation with arm movement
- Pain aggravation when lying on the side of involvement
- Pain may occur with neck flexion in the supine position
- Posterior dislocation may lead to dyspnea, stridor, dysphagia, or upper limb paraesthesia
Physical Examination
- Swelling or prominence at the medial end of the clavicle
- Tenderness on palpation over the sternoclavicular joint
- May have local ecchymosis
- Pain aggravation with shoulder abduction, flexion, or horizontal adduction
- Pain aggravation with resisted neck flexion
- Shoulder special tests may aggravate pain (e.g., Painful Arc and Acromioclavicular Crossover tests)
Imaging
Plain radiography may be used to demonstrate widening of the joint or clavicular dislocation. Computerised Tomography (CT) may be required in cases of posterior dislocation to better evaluate mediastinal structures.
Red Flags
The following are examples of “red flags” for patients presenting with trauma-induced chest pain:
- History of a significant injury
- Severe pain
- Unrelenting pain
- Nocturnal pain or pain at rest
- Fever
- Deformity
- Large joint swelling
- Significant loss of range of motion
- Significant neurological impairment (suggestive of a space-occupying lesion)
- Severe tenderness on palpation or severe pain with any examination procedure
- Dyspnea, stridor, dysphagia, or upper limb paresthesia
If any “red flags” are identified during history taking and clinical examination, referral for urgent medical evaluation and further investigation is warranted.
Management
If no red flags are identified or further investigations do not reveal any contraindications to treatment, management of the condition may begin.
The management approach outlined below is based on published materials (see the References section at the end of this web page) and the clinical experience of the authors of this course. This should not be interpreted as a prescriptive guide to the treatment of this or any other condition. The use of this content is subject to the Disclaimer found at the bottom of this web page.
The following suggestions for therapeutic intervention will depend on the extent of the injury and the stage of recovery.
Conservative Therapy
- Correction of joint dysfunction with emphasis on the shoulder and spine
- Management of any associated myofascial pain syndrome
- Electrotherapy modalities
- Shoulder support (e.g., arm sling, figure-of-eight brace)
- Home advice including activity modification, rehabilitation exercises, and stretches (see below)
Home Advice
- Apply ice over the affected region for about 10 minutes, several times a day for pain control. Ice can be applied as often as every hour.
- Avoid aggravating activities.
- When pain allows, perform muscle strengthening and stretching exercises.
- When it is time to resume activities, initially perform these for only short periods.
Differential Diagnosis
Other conditions that are considered in the differential diagnosis of upper anterior chest pain include:
- Tietze Syndrome
- Sternalis Muscle Myofascial Pain Syndrome
- SCM muscles strain
For Patients
Patient Information Sheet
- Provide information to the patient about their condition to improve their understanding and enhance compliance (see the downloadable ready-to-use Patient Information Sheet below).
- In our experience, patients who are well informed about their condition are more likely to comply with the recommended management strategy, achieve good outcomes, become loyal patients, and recommend their family and friends to seek treatment.
- To view, download or print the Patient Information sheet, simply click on the image below.
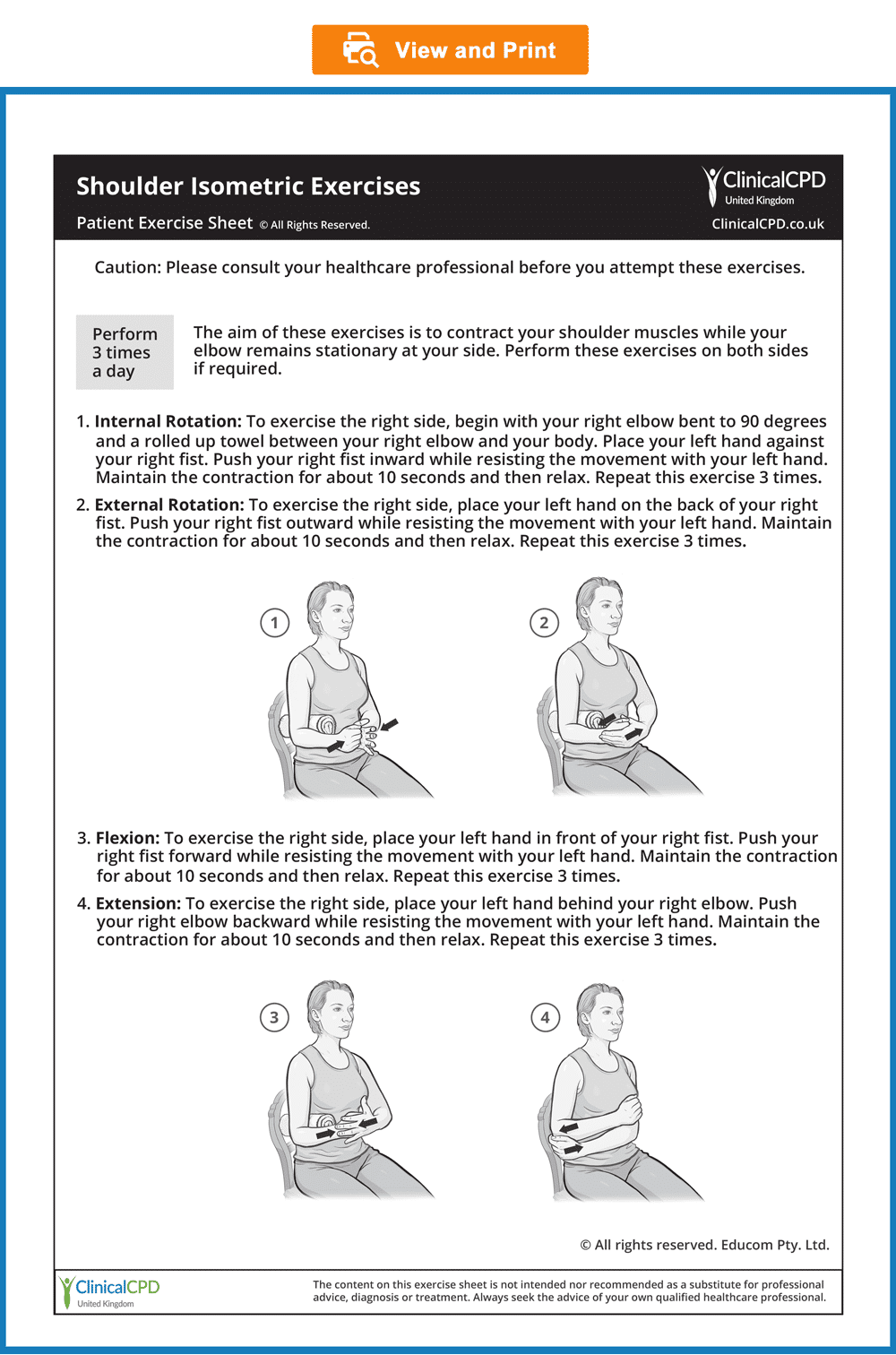
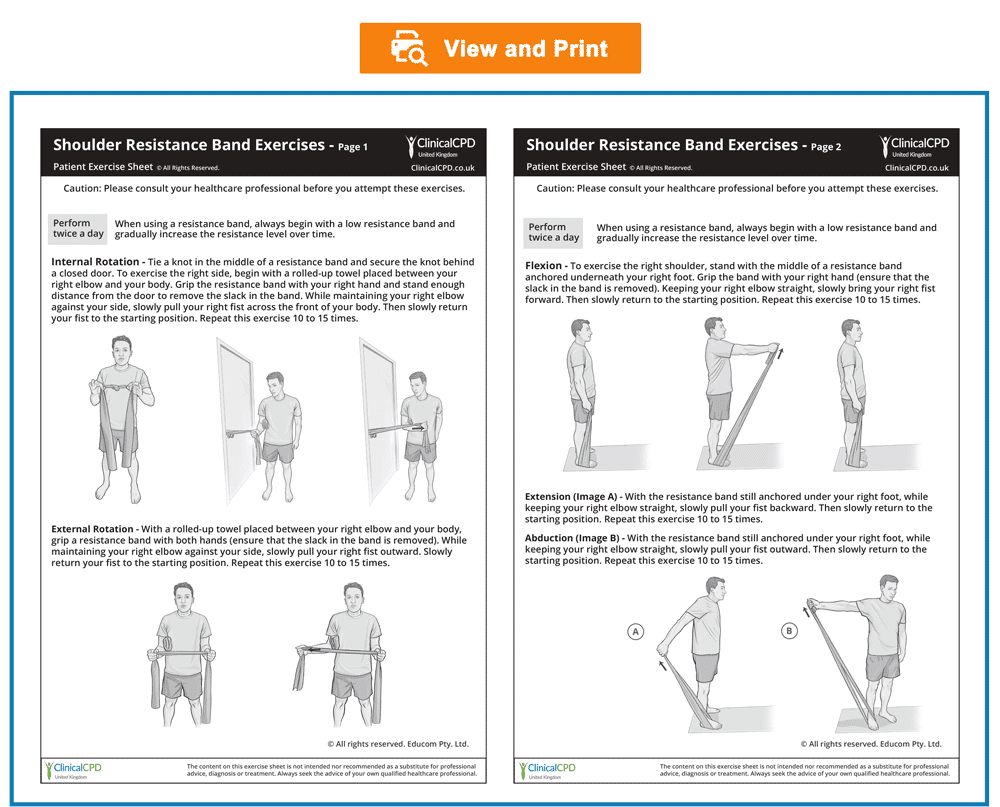
Patient Exercise Sheets
- When appropriate, the patient should gradually begin doing exercises at home.
- Always recommend warm-up activities before commencing specific exercises. Warm-up activities include simple limbering movements or prescribed strength exercises at light loads.
- Instruct your patients to perform any strengthening exercises before they perform any stretching exercises.
- Always instruct your patients to use caution when performing their rehab exercises in order to avoid overloading, overstretching, or any undue pain.
- Emphasise that they should stop any exercises that cause them concern and seek your advice at the earliest opportunity
- To view, download or print the Patient Exercise Sheet, simply click on the image below.
Sample Letters
Sample Referral Letter for Red Flags
- If any “red flags” are identified during history taking and/or physical examination, consideration should be given to referring the patient for urgent medical evaluation and further investigation to rule out serious conditions including infection, fracture, dislocation, or tumours before any treatment can commence.
- For your convenience, we have produced a sample referral letter which is available for download below. You are welcome to copy and paste the text from the sample letter into your own letters and then add your own text to include additional details as required.
Sample Co-Management Letter
- When your clinical evaluation does not reveal any “red flags” but you decide that the patient would benefit from co-management by another practitioner, a referral letter explaining your clinical approach and recommending their involvement in the patient’s management is warranted.
- For your convenience, we have produced a sample letter which is available for download below. You are welcome to copy and paste the text from the sample letter into your own letters and then add your own text to include details such as the clinical presentation, diagnosis, treatment plan, and treatment goal.
Sample Courtesy Letter
- When your clinical evaluation does not reveal any “red flags” and there is no need for a referral, you should consider writing a courtesy letter to your patient’s medical practitioner (with the patient’s consent). In this letter, you can advise them that you have commenced treatment for the patient and demonstrate your professional knowledge, range of clinical skills, and willingness to collaborate with the medical practitioner. In our experience, this approach has been effective in improving awareness of the range of treatment modalities you can provide and encourages the medical practitioner to refer new patients.
- For your convenience, we have produced a sample letter which is available for download below. You are welcome to copy and paste the text from the sample letter into your own letters and then add your own text to include details such as the clinical presentation, diagnosis, treatment plan, and treatment goals.
Patient’s History
In the sections below, you are provided with case history information. The material presents a systematic approach to performing a focused and relevant case history in order to narrow down the possible causes for the patient’s complaint. As you read the following material, you are encouraged to identify whether all the required elements of history taking have been adequately covered.
Who is the patient and where is the pain?
When was the onset and what caused the onset?
Your patient is a 23-year-old university student who presents with acute right shoulder and anterior chest pain following an injury he sustained while participating in a wrestling match three days earlier. He says that he was thrown onto his right side, causing his right shoulder to strike against the floor pushing it backwards and inward. He immediately felt pain in the shoulder that extended across the front of his chest to the base of his throat. To indicate the location of his pain he points to the medial end of his right clavicle.
Analysis: Anterior chest pain in the location that the patient described could be caused by a number of conditions including:
- Clavicular fracture
- Sternoclavicular joint sprain or dislocation
- Upper rib or sternal fracture
- Muscle strain (e.g., pectoralis major, SCM, subclavius)
What are the pain characteristics?
What are the aggravating and relieving factors?
What has been the course of the pain?
He describes his pain as a dull ache at rest, rating it as a 4 out of 10 in intensity with sharp exacerbations on right shoulder movement producing pain intensity of 8 out of 10. The pain worsens when he lies on his right side or when he lifts his head from the pillow when lying on his back. The pain is relieved by applying an ice pack to the area. He says that the pain has eased slightly since the onset.
Analysis: The dull ache with sharp exacerbation on shoulder movement and the aggravation of pain when lying on the right side or when lifting the head suggest local joint injury or fracture. The improvement with rest further suggests that his pain is arising from a mechanical origin. The improvement with the application of ice may indicate an inflammatory process or simply reflect an analgesic effect.
He says that he has tried to avoid activity with his right arm since the onset and that a friend with some first aid experience made him a sling, both of which have provided significant pain relief. He has also found that the application of ice directly over the pain site gives him significant, albeit temporary, pain relief.
The improvement with reduced activity and support as well as the use of ice all confirm that his pain is arising from a local structural injury rather than being a referred pain from a distal site. The improvement with the application of ice may suggest an inflammatory process or simply reflect an analgesic effect.
Are there any associated symptoms?
The patient does not report any associated symptoms or concerns.
Analysis: When patients present with chest pain in association with trauma it is important to look for evidence of fracture with possible mediastinal injury. Therefore the patients should be screened for symptoms such as painful respiration, dyspnea, or dysphagia.
Is there a past history that is relevant to the current complaint?
He reports that he has had several injuries in the past resulting from wrestling matches, including an injury to his right shoulder that produced pain at the ‘tip’ of his shoulder. He says that this occurred about six months ago but quickly resolved with rest and the use of ice.
Analysis: His past history suggests a different injury from the one he is currently presenting with. It is possible however that the previous trauma predisposed him to his current complaint.
Are there any “red flags”?
The patient is asked the following questions in order to identify any “red flags” that could indicate serious pathology. Even if the patient has already provided information in the case history that relates to these questions, it is recommended that they are readdressed to ensure a thorough exploration.
- Do your symptoms disappear even for a short time? “Not really. But I have less pain when I’m not moving my shoulder.”
- Does the pain wake you up at night? “Yes, if I sleep on my right side or lift my head from the pillow.”
- Have you recently had any fever, chills or night sweats? “No.”
- Have you lost any weight recently? “No.”
- Do you have any breathing difficulties or difficulty swallowing? “No.”
- Do you have a history of cancer, respiratory disease or heart disease? “No.”
Analysis: The persistent nature of his pain may be a red flag indicating a serious injury such as a fracture.
What is the list of possible causes for the patient’s complaint?
Based on the available history, the initial list of possible causes for the patient’s complaint includes:
- Clavicular fracture
- Sternoclavicular joint sprain or dislocation
- Upper rib or sternal fracture
- Muscle strain (e.g., SCM, subclavius, pectoralis major)
Reflection Points
Please stop and take a moment to consider whether the main requirements of an adequate and relevant patient history taking have been fulfilled. Are there any additional questions you would have asked and, if so, why?
Before the physical examination findings are presented below, please reflect on what physical examination procedures you would perform to adequately evaluate this patient.
Performing Physical Examination
In the sections below, you are provided with examples of physical examination findings for this patient. The material presents a systematic approach to performing a focused and relevant physical examination in order to narrow down the possible causes for the patient’s complaint. The material also provides ongoing clinical reasoning and analysis of the findings. As you read the following material, you are encouraged to identify whether the essential elements of physical examination have been adequately covered.
Vital Signs
His vital signs are within normal limits.
Inspection
On inspection, there is a localised area of prominence at the medial end of the right clavicle but no apparent ecchymosis (bruising). The clavicular contours are similar on both sides with no evidence of deformity.
Analysis: The localised prominence at the medial end of the right clavicle could be caused by swelling of the sternoclavicular joint, anterior displacement of the sternal end of the clavicle or by epiphyseal separation with displacement. The absence of ecchymosis does not rule out serious damage. The normal contour of the clavicles rules out the possibility of a displaced fracture.
Range of Motion
Active and passive shoulder range of motion is assessed in all directions and result in pain in the region of the right sternoclavicular joint. The pain is most pronounced when horizontal adduction is performed actively and passively. This movement also causes the medial end of the right clavicle to slightly displace forward.
On active abduction of the right shoulder, he experiences pain at about 90 degrees of elevation. The pain increases as the arm is further elevated, with pain reaching its maximum at the end of the range.
Analysis: His localised pain on active and passive shoulder range of motion strongly indicates sternoclavicular joint involvement. Pain production on horizontal adduction and forward displacement of the medial clavicle further confirms sternoclavicular joint involvement with instability.
Assessing for pain on shoulder abduction is commonly referred to as the Painful Arc test. This test is typically used to assess for rotator cuff disorders including Shoulder Impingement Syndrome. However, it can provide evidence for other conditions affecting the shoulder region and neck. In this case, the location and pattern of pain arising from his shoulder abduction indicate a primary injury to the sternoclavicular joint. Please watch the video below if you wish to see how the Painful Arc test is performed.
Muscle Strength Tests
Resistance testing of the right pectoralis major, of right shoulder protraction, and of neck flexion all cause an aggravation of the patient’s pain.
Analysis: These findings reinforce the involvement of the sternoclavicular joint as each of these tests would either load the joint or place strain on the muscles that attach to the sternoclavicular joint.
Palpation
On palpation, there is marked tenderness and some swelling over the right sternoclavicular joint but no evidence of anterior or posterior clavicle displacement. Palpation along the length of the diaphysis of the clavicle produces no tenderness, although there is mild tenderness immediately beneath the clavicle from its midpoint to the medial end.
Analysis: The marked tenderness and swelling suggest the involvement of the sternoclavicular joint. Tenderness immediately below the right clavicle could indicate involvement of either the pectoralis major or the subclavius muscles. The lack of displacement helps to rule out anterior or posterior dislocation.
Neurological Examination
A neurological screening examination of C5 to T1 nerve roots is performed and is found to be normal.
Analysis: Whenever there is trauma involving the sternoclavicular joint there is the possibility of injury to the brachial plexus. Therefore, a neurological screening examination of the C5 to T1 nerve roots is warranted. The absence of findings, in this case, helps to rule out the involvement of the brachial plexus. Another assessment that could be performed is one of the Upper Limp Tension tests. Please watch the videos below if you wish to see how a neurological screening examination for C5 to T1 nerve roots and one of the Upper Limb Tension tests are performed.
Reflection Point
Given the patient’s history and examination findings up until this point, please stop and take a moment to consider which special tests should be performed to further evaluate this patient.
Special Tests
The Acromioclavicular Crossover test is performed and results in significant pain at the right sternoclavicular joint.
Analysis: The Acromioclavicular Crossover test is primarily designed to test the acromioclavicular joint but can be expected to also produce a compressive load at the sternoclavicular joint. The result of this test reinforces the involvement of the sternoclavicular joint. Please watch the video below if you wish to see how the Acromioclavicular Crossover test is performed.
Reflection Point
Please stop and take a moment to consider whether all the elements of an adequate and relevant physical examination have been completed for this patient. Are there any additional procedures you would have performed and, if so, why?
Imaging
Plain radiography is performed and demonstrates a slight sternoclavicular joint space widening on the right.
Analysis: The radiographs confirm the presence of the sternoclavicular joint injury.
Diagnosis
Acute type II right sternoclavicular joint sprain.
References and Suggested Further Readings:
Alexander Van Tongel. Sternoclavicular joint injuries: a literature review. Muscles Ligaments Tendons J. 2011 Jul-Sep; 1(3): 100–105.
Bahk S, Kuhn E, Galatz M, Connor M, Williams R. Acromioclavicular and sternoclavicular injuries and clavicular, glenoid, and scapular fractures. J Bone Joint Surg Am. 2009 Oct;91(10):2492–2510.
Koehler S. Acromioclavicular joint injuries. www.uptodate.com
Renfree J, Wright W. Anatomy and biomechanics of the acromioclavicular and sternoclavicular joints. Clin Sports Med. 2003;22(2):219.
Disclaimer: The Clinical CPD™ website (including the text, graphics and videos that appear on the clinicalcpd.co.uk) are designed to offer users general health information for educational purposes only. The general health information furnished on this site is not intended to replace personal consultation with a qualified healthcare professional. You must always seek the advice of a healthcare professional for questions related to your disease, disease symptoms, and appropriate therapeutic treatments.
Copyright © Educom Pty Ltd: All material on this website (including the text, graphics, videos and downloadable files) are owned by or licensed to Educom Pty Ltd and is subject to copyright and other intellectual property rights under international conventions.
Quiz: This concludes the learning material for this unit. You may review the material or take the multiple-choice quiz for this unit now or at a later time. The quiz for this unit must be completed before you can access the next unit in this course. You can attempt the quiz as many times as you need to achieve a pass mark of at least 60%.
To take the quiz click the button below.